12-Lead ECG Placement Guide with Illustrations
What is Electrocardiogram
 As a non-invasive yet most valuable diagnostic tool, the 12-lead ECG records the heart's electrical activity as waveforms.
As a non-invasive yet most valuable diagnostic tool, the 12-lead ECG records the heart's electrical activity as waveforms.
When interpreted accurately, an ECG can detect and monitor a host of heart conditions - from arrhythmias to coronary heart disease to electrolyte imbalance.
Since the first telecardiogram recorded in 1903, huge strides have been made in the recording and interpretation of ECG. Today, the 12-Lead ECG remains a standard diagnostic tool among paramedics, EMTs, and hospital staff.
Contents
The 12-Lead ECG
A 12-lead ECG paints a complete picture of the heart's electrical activity by recording information through 12 different perspectives. Think of it as 12 different points of view of an object woven together to create a cohesive story - the ECG interpretation.

These 12 views are collected by placing electrodes or small, sticky patches on the chest (precordial), wrists, and ankles. These electrodes are connected to a machine that registers the heart's electrical activity.
Who Should Have a 12-Lead ECG
The main purpose of the 12-lead ECG is to screen patients for possible cardiac ischemia. It helps EMS and hospital staff to quickly identify patients who have STEMI (ST elevation myocardial infarction or in other words, heart attack) and perform appropriate medical intervention based on initial readings.
12-Lead ECG Electrode Placement
To measure the heart's electrical activity accurately, proper electrode placement is crucial.
In a 12-lead ECG, there are 12 leads calculated using 10 electrodes.
Chest (Precordial) Electrodes and Placement

» V1 - Fourth intercostal space on the right sternum
» V2 - Fourth intercostal space at the left sternum
» V3 - Midway between placement of V2 and V4
» V4 - Fifth intercostal space at the midclavicular line
» V5 - Anterior axillary line on the same horizontal level as V4
» V6 - Mid-axillary line on the same horizontal level as V4 and V5
Limb (Extremity) Electrodes and Placement

» RA (Right Arm) - Anywhere between the right shoulder and right elbow
» RL (Right Leg) - Anywhere below the right torso and above the right ankle
» LA(Left Arm) - Anywhere between the left shoulder and the left elbow
» LL (Left Leg) - Anywhere below the left torso and above the left ankle
Additional notes on 12-lead ECG Placement:
- The limb leads can also be placed on the upper arms and thighs. However, there should be uniformity in your placement. For instance, do not attach an electrode on the right wrist and one on the left upper arm.
- For female patients, place leads V3-V6 under the left breast.
- Do not use nipples as reference points in placing electrodes for both men and women as nipple locations vary from one person to another.
The 12 Lead Groups

A lead is a glimpse of the electrical activity of the heart from a particular angle.
Put simply, a lead is like a perspective. In 12-lead ECG, there are 10 electrodes providing 12 perspectives of the heart's activity using different angles through two electrical planes - vertical and horizontal planes.
Vertical plane (Frontal Leads):
By using 4 limb electrodes, you get 6 frontal leads that provide information about the heart's vertical plane:
- Lead I
- Lead II
- Lead III
- Augmented Vector Right (aVR)
- Augmented Vector Left (aVL)
- Augmented vector foot (aVF)
Leads I, II, and III require a negative and positive electrode (bipolarity) for monitoring. On the other hand, the augmented leads-aVR, aVL, and aVF-are unipolar and requires only a positive electrode for monitoring.
Einthoven's Triangle

The Einthoven's triangle explains why there are 6 frontal leads when there are just 4 limb electrodes.
The principle behind Einthoven's triangle describes how electrodes RA, LA and LL do not only record the electrical activity of the heart in relation to themselves through the aVR, aVL and aVF leads. They also correspond with each other to form leads I (RA to LA), II (RA to LL) and III (LL to LA).
As a result, they form an equilateral triangle. Hence it's called the Einthoven's triangle, named after Willem Einthoven who invented the first practical ECG.
Keep in mind that RL is neutral (also known as point zero where the electrical current is measured). RL doesn't come up in ECG readings, and is considered as a grounding lead that helps minimize ECG artifact.
Horizontal Plane (Transverse Leads)
By using 6 chest electrodes, you get 6 transverse leads that provide information about the heart's horizontal plane: V1, V2, V3, V4, V5, and V6.
Like the augmented leads, the transverse leads are unipolar and requires only a positive electrode. The negative pole of all 6 leads is found at the center of the heart. This is calculated with the ECG.
Patient Positioning for 12-Lead ECG Placement
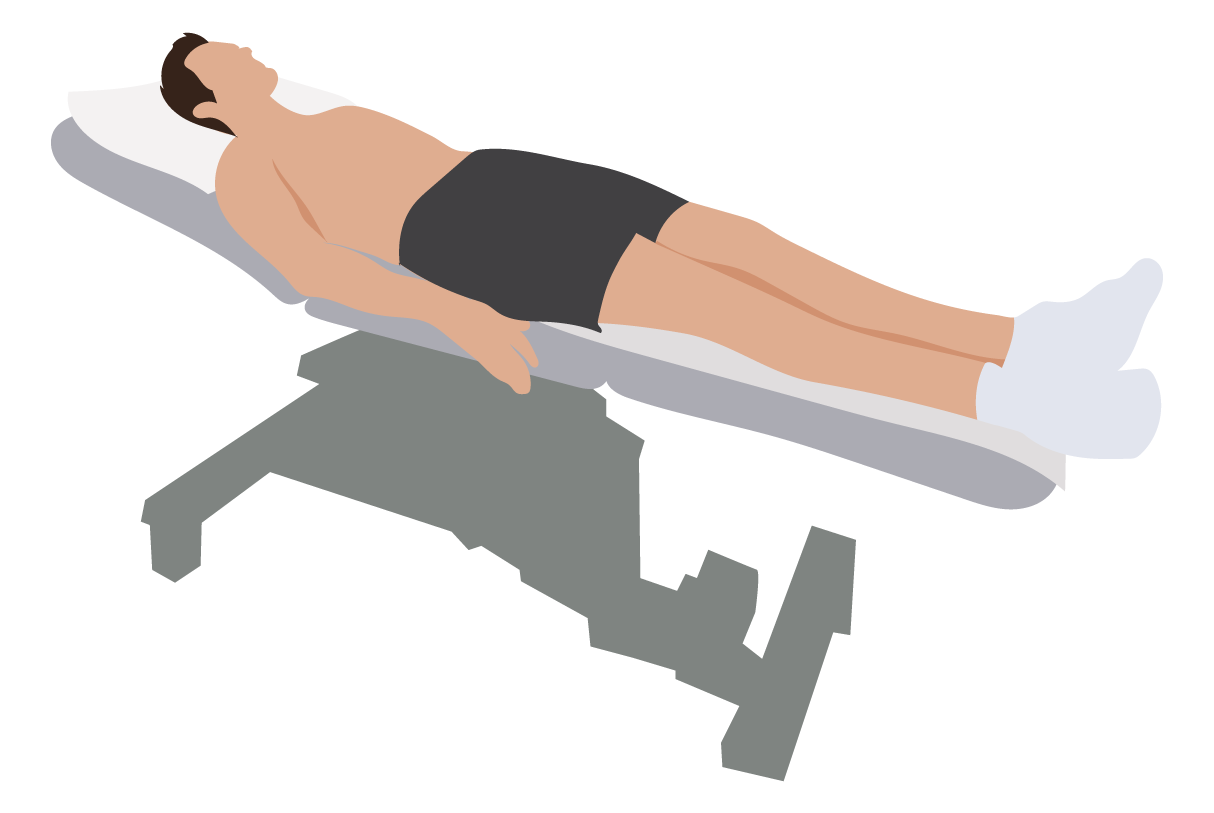
- Ensure that electronic devices (e.g. smartphone) are removed from the patient. These devices can produce artifact (interference) and cause problems with the readings.
- Place patient in supine or Semi-Fowler's position. If both positions are impossible, you can perform ECG with the patient in a more elevated position.
- With arms lying flat on the side, ask the patient to relax the shoulders and keep the legs uncrossed.
- For patients that do not fit comfortably on the bed or exam table due to size, ask them to cross their arms on their stomach to reduce muscle tension and movement.
- Unless you're performing a stress ECG test, ask the patient to lie still and quietly until the test is done.
How to Reduce Significant Artifact
A slight ECG artifact is not uncommon. However, you can reduce further interference through the following steps:
- Switch off non-essential electrical devices and equipment within the vicinity if possible.
- Check for cable loops and avoid running cables adjacent to metallic objects as they can affect the signal.
- Inspect wires and cables for cracks or breaks. Replace as needed.
- If possible, use surge suppressors with the power supply.
- Ensure that filters and preamplifiers are appropriately adjusted.
- Ensure securely connection between patient cable and the ECG device. Double check for gaps between connectors.
Skin Preparation

- Skin should be dry, hairless, and oil-free. Shave hair that can possibly impede electrode placement. Electrodes should have full contact with the patient's skin.
- For better electrode adhesion and oil-free skin, rub the area with an alcohol prep pad or gauze paid with benzoin tincture.
- Reduce electrical resistance minus the skin redness with 5 to 10 gentle strokes. This will help ensure that the heart's electrical signals are transmitted to the electrodes.
- Promote an environment that prevents the patient from sweating profusely.
Electrode Application
Exact placement of each electrode on the patient is important. Incorrect placement can lead to false or misleading diagnosis.

- Make sure the electrode conducting gel is fresh and adequately moist. A dry electrode with inadequate gel reduces the conduction of the ECG signal.
- Often, electrode gel dry-out is a result of incorrect storage. Store electrodes as instructed by manufacturer and do not remove from their pouch until they're ready for use.
- Do not place electrodes on skin over bones, incisions, irritated skin, and body parts where there is lots of possible muscle movement.
- Use electrodes of the same brand. Using different brands with dissimilar composition can hinder an accurate ECG trace.
ECG Variations
Apart from the standard 12-lead ECG, other variants include:
3-Lead ECGA 3-Lead ECG uses 3 electrodes that are labeled white, black, and red. These colors are not universal as two coloring standards exist for the ECG (discussed below). These 3 leads monitor rhythm monitoring but doesn't reveal sufficient information on ST elevation activity.
5-Lead ECGA 5-Lead ECG uses 4 limb leads and 1 chest lead. It helps improve ST elevation readings but it's still inferior to the 12-lead ECG.
Color Coding Standards for the 12-Lead ECG
Currently, there are two color coding standards for 12-lead ECG:
- IEC (International Electrotechnical Commission) system
- AHA (American Heart Association) system

If you're using AHA's system, use this mnemonic to easily recall limb electrode placement:
- smoke over fire (black lead above the red lead)
- snow over grass (white lead above the green lead)
ECG Best Practices:
- Always protect the patient’s privacy and dignity by draping with a sheet to minimize exposure.
- Lead placement and patient positioning should be the same for subsequent ECGs on any individual patient.
- During the procedure, record any clinical signs (e.g. chest pain) in the notes or on the ECG tracing itself.